Upgrading air management systems for hospital laboratories

With many hospitals now addressing longer waiting lists, pressure on laboratory facilities has never been so intense, says Ian Thomas of TROX UK
Some institutions have extended their working hours to meet demands, whilst many laboratory technicians have altered shift patterns to facilitate social-distancing. As a result, today’s hospital laboratory facilities need to be more flexible than ever before, to enable scientists from different disciplines to work alongside one another safely, optimising usage of the available equipment. In addition, NHS Trusts are faced with significant increases in running costs relating to laboratories.
This article looks at some of the key challenges facing hospital laboratories, and suggests approaches to the upgrading of air management systems to assist in tackling these issues. Well-designed ventilation systems are crucial to enable clinicians and laboratory technicians to work more effectively and productively without compromising health and safety. In addition, improving the efficiency of the air management systems can help NHS Trusts to regain control over spiralling energy costs of laboratories.
Safety first
Increasingly hospital sites are being designed with multiple functions, combining clinical work with medical research. Many sites are also university hospitals, involving aspects of teaching and learning. To enable these multiple operations to be carried out safely within a single building, the design of the air management scheme needs to accommodate multiple zones with different containment levels. This, in turn, determines the optimum supply and extraction strategy and identifies the appropriate filtration requirements.
The Quadram Institute building at the Norwich Research Park, for example; needed an air management scheme which would enable multiple clinical and research operations to be accommodated within a single new build development. The Quadram Institute brings together the former Institute of Food Research, the University of East Anglia Clinical Research Facility and the gastrointestinal endoscopy unit of Norfolk and Norwich University Hospital to conduct translational research and clinical care. It houses around 300 researchers, as well as clinicians and support staff. In addition, as the largest unit of its type in Europe, it is designed to welcome up to 40,000 endoscopy outpatients each year. The building provides distinct accommodation for each department, as well as shared office space, meeting rooms and amenities to encourage interaction between all user groups.
The Quadram Institute includes Containment Level 2 and 3 Laboratories, as well as being a major Clinical Trials facility and a centre of excellence for endoscopy. This necessitated an added requirement for control and repeatability of air management conditions, in addition to the wider requirements for energy efficiency.
During the design phase, wind tunnel testing was carried out to determine safe fume efflux parameters for the scheme. The air terminal device requirements of different zones in the building were also analysed to determine the best possible designs of grilles and diffusers to maintain the optimum safe and comfortable working environment for researchers, staff and patients. To account for the specific research operations carried out in separate departments across the site, the building services professionals worked in collaboration with clinical experts to determine the most appropriate HEPA filter cells and diffusers for the different zones of the site.
The resulting air management system for the Quadram Institute ensures that supply and extraction of air is optimised automatically in each laboratory to maintain safe working environments. Specific room pressure control capabilities are installed for the Containment Level 3 labs, and volume offset tracking controls for the Containment Level 2 spaces.
The air management requirements for the Containment Level 3 suite were particularly challenging. For this critical zone, the air management system controls a pressure cascade, within which laboratories are controlled at larger negative pressures than the adjacent circulation spaces serving them, to ensure there can be no reversal of airflow under normal operational conditions. The suite also has an automated ventilation sequence that allows ventilation shut down, fumigation and purge of labs in a number of combinations to allow maximum flexibility. This automated ventilation sequence works by switching the air management system between different flow rate set points and pressure set points to achieve the desired ventilation strategy.
Tackling energy costs
In addition to the needs for safety and flexibility, NHS Trusts must accommodate the demands placed on hospital laboratories against a backdrop of spiralling energy costs. The energy consumption of laboratories is often more than three or four times that of offices on a square metre basis. This can mean that laboratory buildings are responsible for between 50% and 80% of the total energy-related (non-residential) carbon emissions of research-intensive universities. Government research facilities, hospitals and private sector laboratories are similarly affected.
The higher energy costs and carbon emissions of laboratories are typically associated with the air supply and extraction requirements of fume cupboards. When sashes of fume cupboards are open, the volumes of air required to maintain a safe working environment for laboratory personnel increase significantly. For example, a 900mm wide cupboard with a maximum sash height of 500mm and face velocity of 0.5 m/s would extract approximately 225 l/s of conditioned air from the room. By contrast, the minimum air volume for a variable air volume fume cupboard would only be around 55 l/s when the sash is closed, saving 170 l/s of conditioned air, whenever the sash is in the down position.
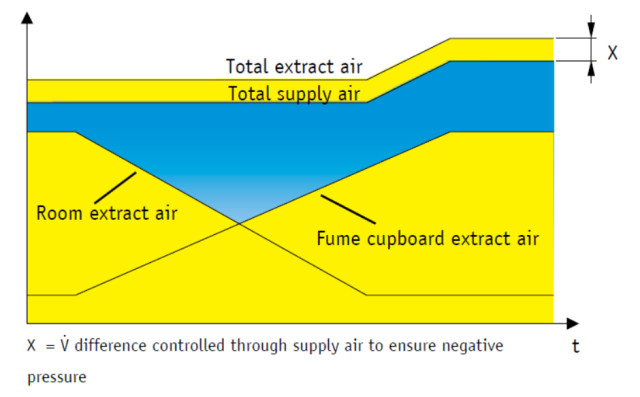
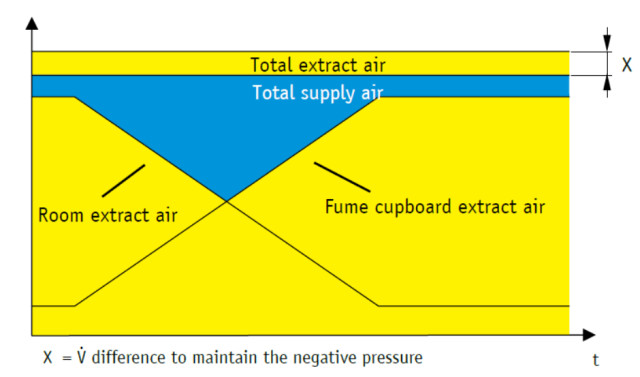
Best practice is to install a room air management system to fully integrate fume cupboard air supply and extraction with the wider air management systems to prevent wastage. The room air management system makes it possible for all input and extract air for the laboratory to be controlled automatically to ensure that the required ventilation strategy and levels of safety are maintained. With this design approach, the supply and extraction of the fume cupboards (or other technical air management devices) is automatically balanced and offset in line with changing requirements, reducing the total supply and extract volumes. For example, if the fume cupboards are open and extracting air, there is not the same requirement for the room system to carry out this process. By scaling down room exhaust air extraction in line with fume cupboard extraction, the room air management system is able to prevent over-supply and extraction of conditioned air from the space, improving energy efficiency significantly. See Figures 1 and 2.
If hospital budgets do not currently permit the installation of a room air management system, there may still be energy reduction measures that you can retrofit to reduce consumption and cost in the short or medium term. Firstly, you could assess whether energy efficiency of the fume cupboards can be enhanced by retrofitting new control technology into the existing cabinets. Secondly, it could be possible to introduce devices to close the sashes of fume cupboards automatically when they are not in use. Automatic systems, based on presence detection, can prevent unnecessary wastage of conditioned air. Thirdly, it might be beneficial to install local cooling or extraction devices such as ventilated down flow tables, canopy hoods or fume exhaust ‘snorkels’. These are capable of reducing loading on the central air conditioning facilities for the site by taking heat away at source.
As hospitals continue to perform their vital roles, effective air management of laboratory spaces can be an important factor in addressing the challenges they face.
Ian Thomas is Product Manager – LabControls at TROX UK